Hello! Well, today I am posting on a Diabetes Education class that I attended on Monday & Tuesday of this week (3/18-19) at Naval Hospital Pensacola. The class was taught mainly by Joyce Robinson and LaNora Glaze whom are both registered nurses and CDE (Community Diabetes Educators). However, guest speakers also played a big part in the program by educating the participants and other important areas of concern regarding Diabetes. The target audience was for pre-diabetic or diabetic patients with type I and type II.
Monday’s agenda:
0800-0815 Welcome & Overview by Joyce
0815-0905 What is Diabetes? by Joyce
0915-1000 Monitoring & Short Term Complications by LaNora
1015-1100 Medications by pharmacist LT Meaghan Horrigan
1110-1200 The Wellness Center by Bob Thomas, MWR Director
Tuesday’s agenda:
0800-0920 What Should I Eat? by Shelley Pino, Registered & Licensed Dietician
0930-1015 Quality of Life by Rikki Vidak, Social Worker at NHP
1030-1120 Long Term Complications by Joyce
1130-1200 Wrap Up/Evaluations by Joyce
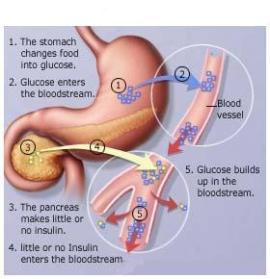
If I explained in detail what all I learned, I’d be writing for 8 hours, so instead I will just give you the basics and some of my favorite parts of the training. On Monday, we covered the basics on Diabetes. A lot of these patients were clueless about their disease and so Joyce explained what happens and what is diabetes? Here is a good photo to describe diabetes:
Understanding Diabetes
The food you eat is digested to be used as fuel. This fuel supplies energy to your body’s cells. When you have Diabetes, the fuel has a hard time entering most cells.
In Depth
The digestive system breaks down food, resulting in a variety of nutrients including a sugar called glucose. Some of the glucose is stored in the liver. Most of it enters the bloodstream and travels to cells to be used as fuel. Glucose needs the help of a hormone (chemical messenger) called insulin to enter most cells. Insulin is made in the pancreas. It is released into the bloodstream in response to meals and the presence of glucose in the blood. Think of insulin as a key. When insulin reaches a cell, it unlocks a doorway into the cell that allows glucose to enter the cell.
Diabetes: Your body may not make enough insulin, or may make none at all. And/or your cells may not respond the right way to insulin in the blood. Either way, this means that glucose ha trouble entering the cells. If it can’t enter the cells, it builds up to a harmful level in the blood stream. This is called high blood glucose or hyperglycemia.
Discussing the Types
When you have type 1 diabetes, the pancreas is not making any insulin at all. Type 1 diabetes most often develops in children. But adults at any age can also get it. People with type 1 usually must take insulin every day in order to get fuel into most cells.
When you have type 2 diabetes, the pancreas may still be making some but not enough insulin. And the cells may not respond to insulin the way they should. This is called insulin resistance. The pancreas may try to overcome resistance by making more insulin. But the pancreas can’t provide the extra insulin needed. People with type 2 diabetes may also need to take insulin, but more importantly- monitor their diet and exercise! Which falls into the next topic of Monitoring your Diabetes…
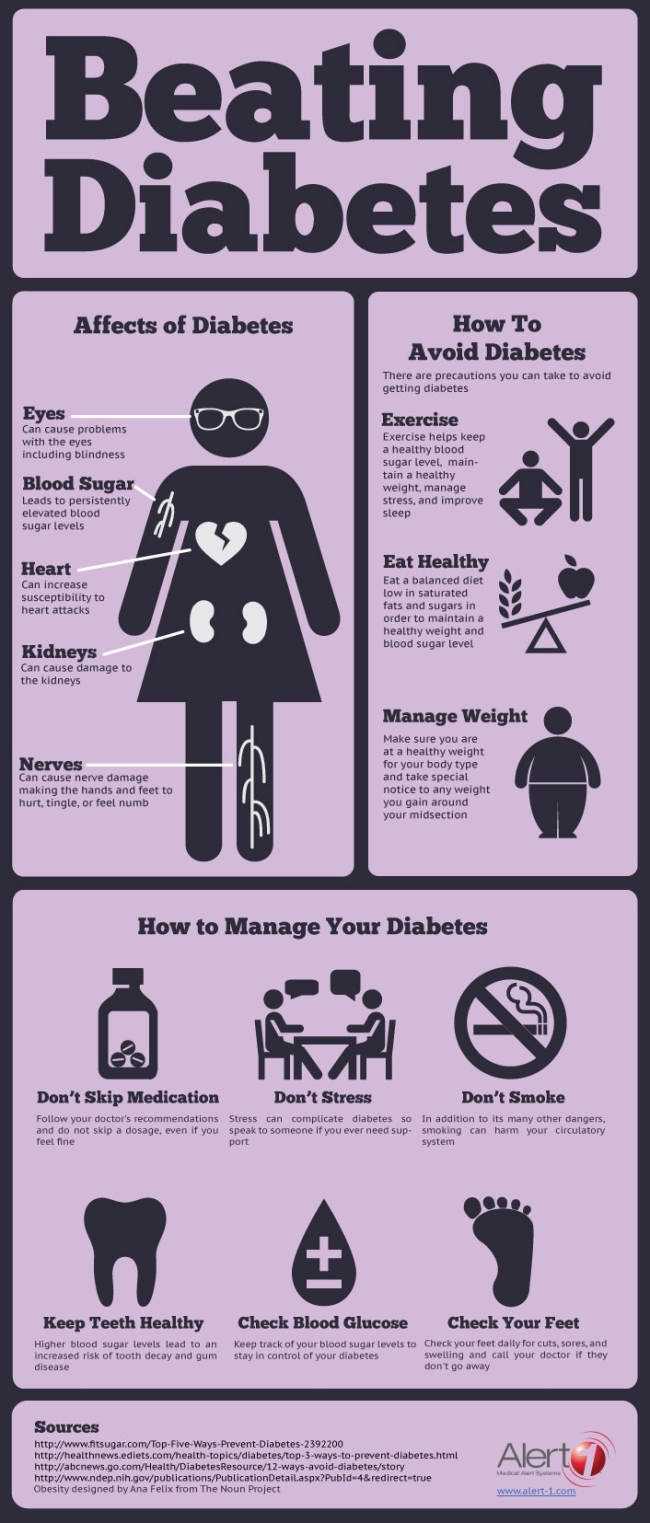
We went over the symptoms associated with Diabetes and what all it can do to your body. Typically those with Diabetes also have other existing issues such as high cholesterol, nerve problems, food allergies, etc. One thing they placed a big emphasis on was self-care and that only you are in charge of how you deal with your Diabetes. It’ all about choices.
Monitoring
Well, most people with diabetes SHOULD have a monitor or reader. This tells them their blood glucose levels. The goal is to keep your blood glucose levels within target range throughout the entire day. You also want to monitor your blood glucose levels after eating certain foods to discover whether or not they spiked your levels so that in the future you can avoid or limit those items from your diet. The target range for pre-meal blood glucose is 70-130mg/dL and <180mg/dL post-meal (or up to 2 hrs after you finish eating). This is helpful when trying to maintain in a healthy target range. While there’s hyperglycemia, there’s also hypoglycemia which means your blood sugar level is dropping too low. This can happen when consuming alcohol and not eating (which is not advised for diabetics because it is hard to diagnose whether they are drunk or having negative symptoms from the diabetes.. very dangerous!).
I’m going to skip over some and talk more about my favorite parts of the class which included of course Nutrition & Fitness 🙂
So, Bob Thomas (who actually did my CPR certification) came and talked to the group on exercise and the important role it plays in controlling your diabetes. Exercise actually helps to lower your blood glucose levels because it burns some of that excess glucose and uses it for energy. He told them all about the different classes available at MWR on base and at the end, he talked to me a little more on shadow/job opportunities. We set up a time to meet and talk more on Friday, so I look forward to that. If I was in desperate need of a job, I would resort to becoming certified in fitness coordinating and taking the ACE exam to do so.
Anyway, moving onto Nutrition. Being that I have been working on a Nutrition Brief for the Army folks the past week, I was anxious to hear Shelley Pino’s lecture on Nutrition. She’s the RD at the Naval Hospital, ex-air force and super fun. She brought all her food demos and we had a good time. Basically, she covered the importance of carbohydrates in the diabetic diet. Carbs are the main source of glucose, therefore it needs to be limited and controlled. She gave them alternatives and healthy food options as well as resources to find diabetic recipes.
Well, that is all I’m going to say for now. I could go on and on about Diabetes! Oh wait, reminds me of one last important thing! 🙂
The A1C is a test that gives an average of the patient’s blood glucose levels over a period of time. Basically, it is advised that the diabetic has an appointment with their doctor every 6 months to review their A1C score and make sure that it is below 7%. Pre-diabetics are considered to be at 6%. The risks for diabetes include: being overweight, a sedentary lifestyle, age (although with the obesity epidemic, children are now being diagnosed), genetics or family history of diabetes, and race (typically the darker skin tones).
Ok, I think that is it. We covered tons of information (actually everything there is to know about Diabetes) in this class. The pharmacist talked about the different medications for diabetes and side effects of each, etc. The social worker gave a good analogy on diabetes by comparing it to a new born baby. When you first have a baby, it’s ALL about the baby. But after a while, it dies down. That’s like being diagnosed with Diabetes. At first, it’s all about the diabetes and you think your life is ruined, however it DOES and WILL get better with control and self-care!
Daily hours: 14
(When I got home, I worked on the Nutrition Brief each day for a total of 6 hours)
Total hours: 230